Learn how symptoms like indigestion or diarrhea may point to Crohn’s disease, what your small intestine does, and why proper health insurance matters in the U.S.
- Something Doesn’t Feel Right—Could It Be More Than Indigestion?
- The Small Intestine—Your Hidden Workhorse
- What Happens When It Breaks Down?
- The Health Insurance You Didn't Know You Needed
- Other Conditions You Shouldn’t Ignore
- Protecting Your Gut—What You Can Do
- When Your Intestine Stops—Understanding Small Bowel Obstruction
- The Insurance Factor—Don’t Risk Facing This Alone
- Elderly at Higher Risk—What to Watch Out For
- Why Insurance Is Your Best Protection
- Why Insurance Is Your Best Protection
Something Doesn’t Feel Right—Could It Be More Than Indigestion?
You might brush off your bloated stomach, occasional diarrhea, or that nagging fatigue as just part of life. Maybe you’ve blamed it on fast food, stress, or poor sleep. But what if your symptoms are trying to tell you something more serious?
“Crohn’s disease is an inflammatory condition that can affect the entire digestive tract—from mouth to anus.”
That’s how Dr. Yoo, a leading pathology professor, opens his discussion on the small intestine, a part of our body that often goes overlooked—until something goes wrong.
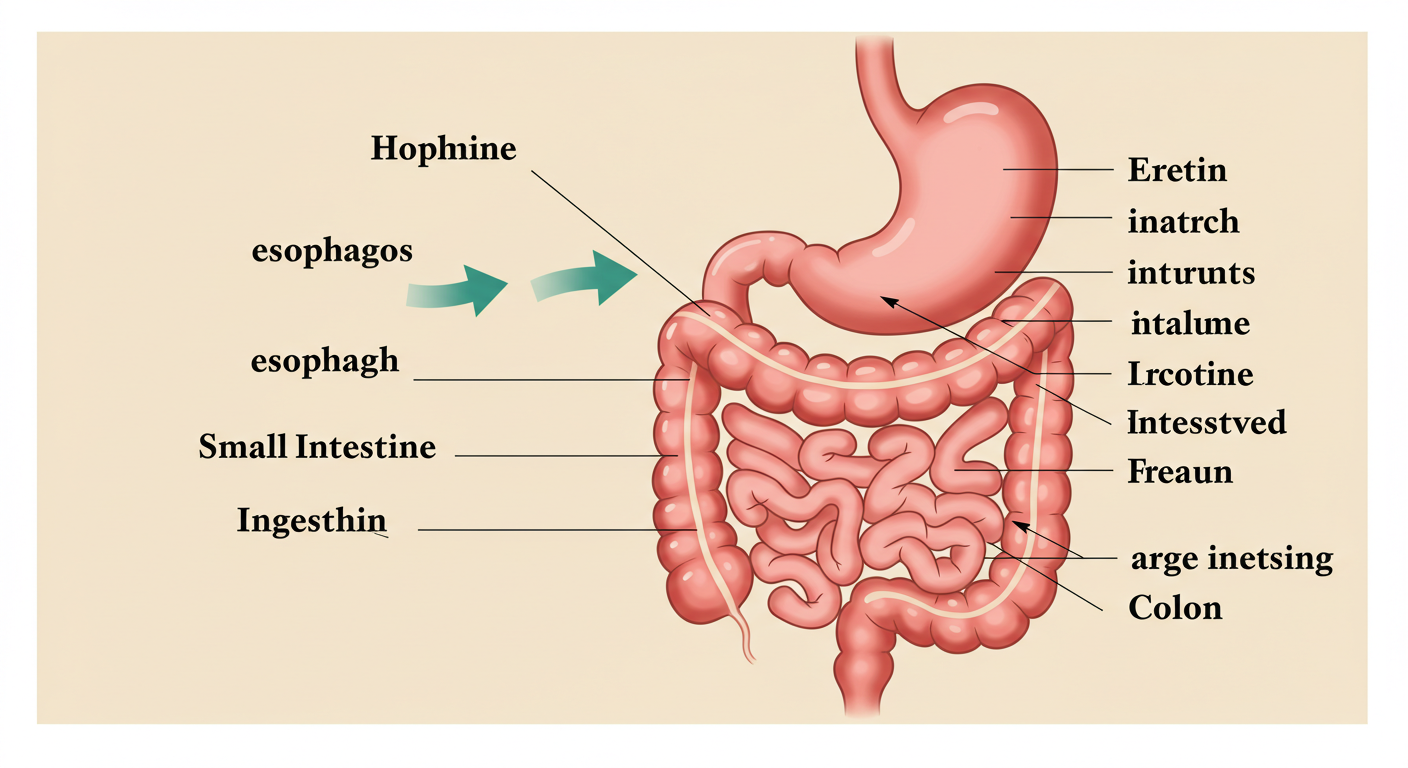
The Small Intestine—Your Hidden Workhorse
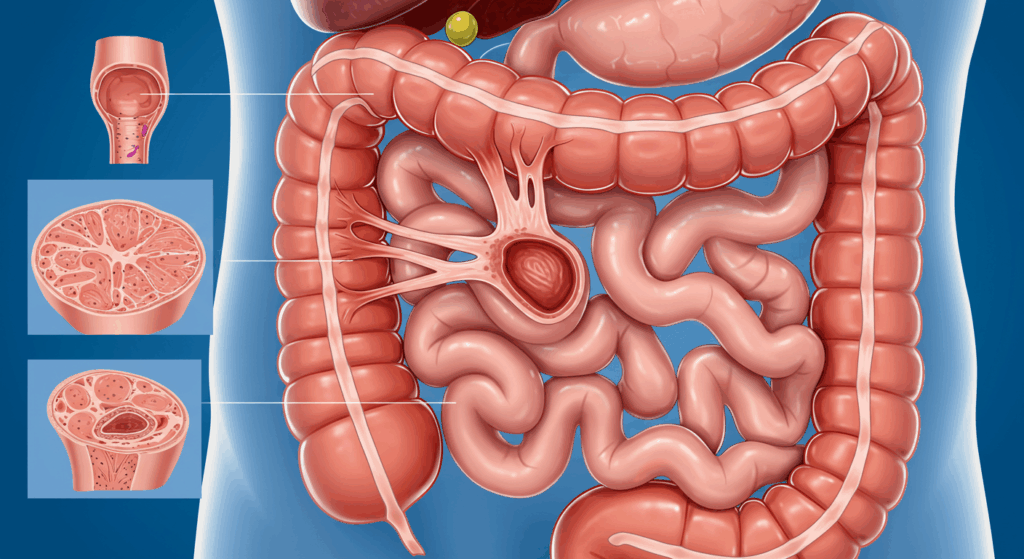
Most people don’t know this, but your small intestine is about 6 to 7 meters long—over 20 feet of tightly coiled digestive powerhouse inside your abdomen. It’s divided into three parts:
- Duodenum : About 30 cm long, this C-shaped segment receives bile and pancreatic enzymes to break down fats, proteins, and carbs.
- Jejunum : Roughly 2.5 meters long, where most absorption begins.
- Ileum : The final 3.5 meters, fine-tuning the absorption of nutrients like B12 and bile salts.
These sections work together through peristalsis (muscle contractions) to mix and push your food forward, while absorbing everything your body needs.
“Without the small intestine, we can’t absorb nutrients. You would slowly starve, no matter how much you eat.”
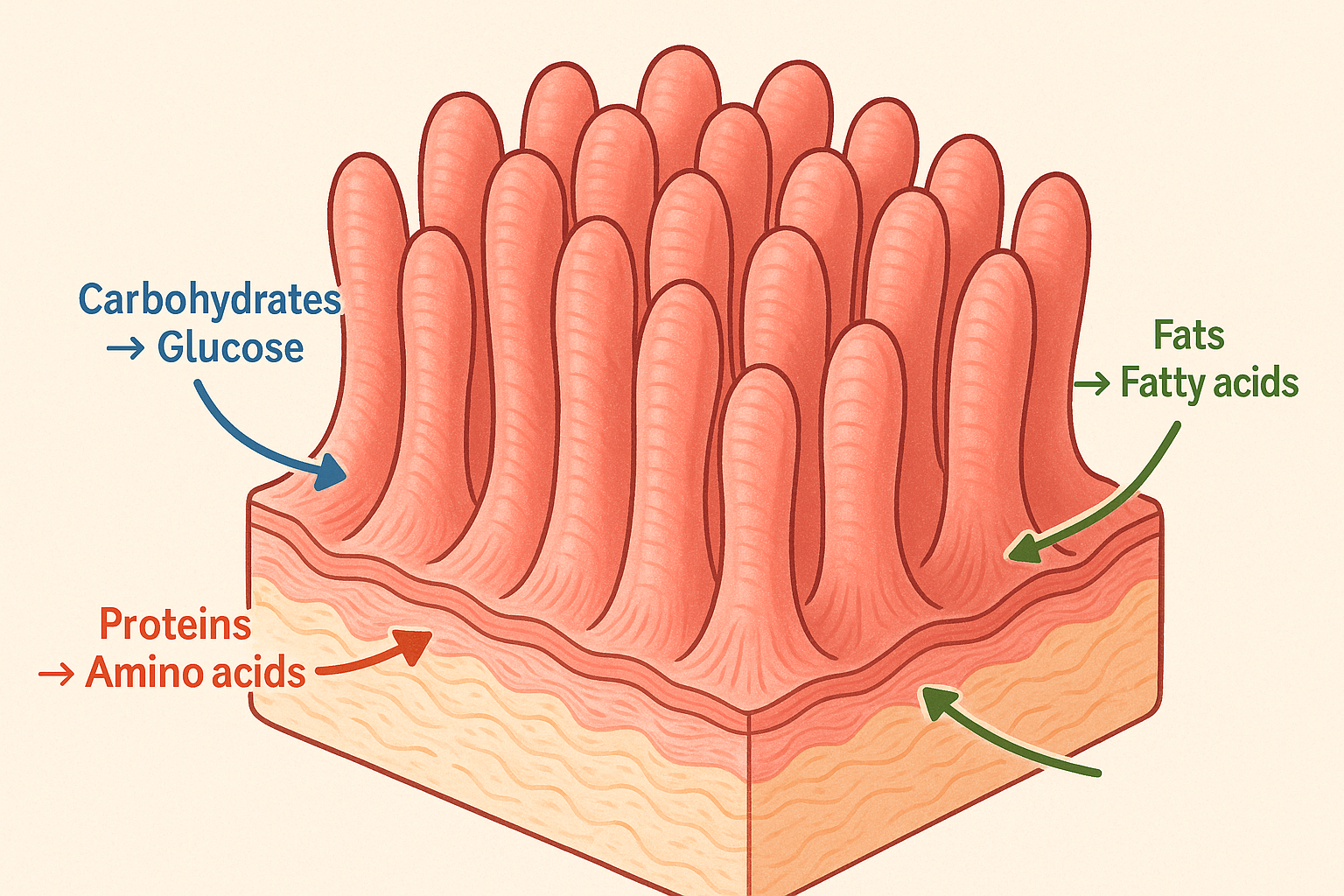
What Happens When It Breaks Down?
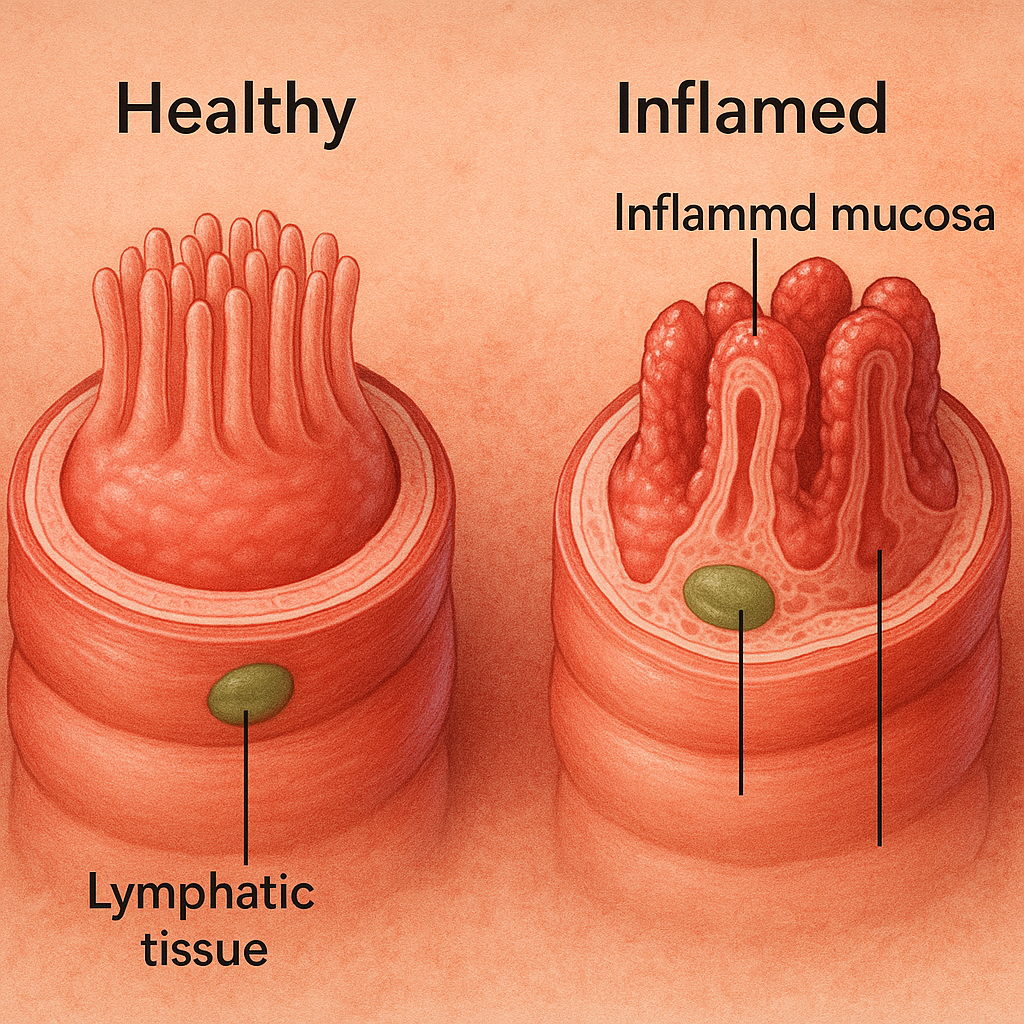
When inflammation hits the small intestine—as it does in Crohn’s disease—the smooth digestion process turns chaotic.
Imagine looking at the intestinal wall under a microscope and seeing immune cells rampaging. The entire lining becomes inflamed and swollen, disrupting nutrient absorption and triggering symptoms such as:
- Chronic diarrhea
- Abdominal pain
- Weight loss
- Extreme fatigue
- Malabsorption of vitamins and minerals
“Crohn’s disease isn’t just about a sore stomach. It’s an autoimmune condition. Your body is attacking your own digestive system.”
The Health Insurance You Didn’t Know You Needed
When Crohn’s disease strikes, the real cost isn’t just discomfort. It’s the medical bills—especially in the U.S., where chronic illness care can be financially devastating.
Why You Need Health Insurance for Crohn’s
Crohn’s often requires:
- Regular endoscopies and colonoscopies
- Immunosuppressants and biologic drugs
- Nutritional therapy and supplements
- Emergency care or intestinal surgeries
- Ongoing consultations with gastroenterologists
A single biologic infusion can cost $5,000–$20,000 without insurance.
“If you don’t have health insurance that covers chronic inflammatory diseases, a Crohn’s diagnosis could bankrupt you.”
📎 Helpful Resource: Crohn’s & Colitis Foundation Insurance Guide
📎 Apply for Health Insurance via Healthcare.gov
Other Conditions You Shouldn’t Ignore
Crohn’s isn’t the only culprit. Other lesser-known but serious small intestine diseases include:
- Celiac Disease: Gluten-triggered immune response damaging the intestine
- Small Bowel Obstruction (SBO): Often from past surgeries causing adhesions
- Small Intestinal Cancer: Still rare but on the rise, especially with chronic inflammation
“I’ve seen cases where a patient ate something sticky like jelly and it clogged an already narrowed intestine from previous surgery. They passed away from small bowel obstruction.”
Protecting Your Gut—What You Can Do
Even without a diagnosis, take these preventive steps seriously:
- Exercise regularly — it stimulates healthy gut movement
- Eat high-fiber diets and stay hydrated
- Avoid self-medicating with unproven “gut detox” kits
- Get screened early if you experience chronic gut symptoms
And most critically:
Make sure your health insurance includes chronic disease management. This can be the difference between sustainable care and financial disaster.
When Your Intestine Stops—Understanding Small Bowel Obstruction
Sometimes, the issue isn’t inflammation—it’s a traffic jam inside your gut.
“Small bowel obstruction happens when the intestine can no longer move its contents forward. This can be due to adhesions from previous surgeries, tumors, or severe inflammation.”
Unlike Crohn’s disease, which slowly builds over time, small bowel obstruction (SBO) can strike suddenly—and it’s often a medical emergency.
What Causes SBO?
- Adhesions (scar tissue) from past abdominal surgeries
- Tumors pressing against or growing into the small intestine
- Hernias or twisted segments (volvulus)
- Inflammatory diseases like Crohn’s that narrow the lumen
- Foreign substances or food blockages (e.g., jelly-like foods, undigested fiber)
Causes of Small Bowel Obstruction
- ⬇️ Previous abdominal surgery → Adhesions (scar tissue)
- ⬇️ Tumors → External pressure or growth into the intestine
- ⬇️ Hernias or volvulus → Twisting of the bowel
- ⬇️ Crohn’s Disease → Chronic inflammation and narrowing
- ⬇️ Food blockages → Sticky substances in narrowed intestines
In extreme cases, this can lead to ischemia (loss of blood flow), necrosis, or death if left untreated.
The Insurance Factor—Don’t Risk Facing This Alone
A small bowel obstruction (SBO) doesn’t just attack your health—it can cripple your finances.
While it’s easy to dismiss abdominal pain as indigestion or constipation, when that pain escalates into vomiting, bloating, and inability to pass gas or stool, you may already be in an emergency.
“Many patients don’t realize the severity until it’s too late. A blocked small intestine is not something you can walk off.”
Once you’re in the emergency room, the medical rollercoaster begins: imaging, IV fluids, nasogastric tubes, and in many cases, immediate surgery.
Here’s what such an episode might cost in the United States:
📊 [Cost Comparison Table — With vs Without Insurance]
| Treatment Item | With Insurance | Without Insurance |
|---|---|---|
| ER Visit + Evaluation | $150 – $500 | $3,000 – $6,000 |
| CT Scan + Diagnostics | $200 – $800 | $2,000 – $5,000 |
| Emergency Surgery | $1,500 – $4,000 | $15,000 – $40,000+ |
| 3–7 Days Hospital Stay | $600 – $1,200/day | $6,000 – $10,000/day |
This is where health insurance becomes your shield.
What Kind of Insurance Do You Need?
Not all plans are created equal. For something like SBO or Crohn’s disease, your plan should cover:
- ER visits
- Surgical procedures
- Inpatient care
- Follow-up visits
- Prescription medications
- Out-of-network emergencies
A Bronze or Silver ACA plan may offer basic protection, but patients with chronic GI issues often opt for Gold tier or PPO plans to minimize out-of-pocket burden.
📎 Compare ACA Health Plans – Healthcare.gov
📎 Crohn’s & Colitis Foundation: Insurance Help
“The problem isn’t just medical—it’s logistical. Without insurance, you may hesitate to go to the hospital at all. That hesitation can cost your life.”
Elderly at Higher Risk—What to Watch Out For
Small bowel obstruction isn’t just a random emergency—it’s often the result of years of accumulated risk, especially in older adults.
“In the elderly, a simple jelly-like food can turn deadly if it gets stuck in a narrowed intestinal passage.”
This scenario isn’t rare. Many elderly patients have undergone past surgeries (like gallbladder removal or hernia repair), which leave behind adhesions—thin strands of scar tissue that can entangle or compress the intestines.
On top of that, reduced mobility, weakened abdominal muscles, and chronic constipation add to the problem.
A Real Case Example
Dr. Yoo recalls a case involving an elderly patient who had a narrowed section of the duodenum (the first part of the small intestine) due to a past surgery. After eating a sticky jelly-based dessert, the man developed a total obstruction and died from complications.
“He ate several packs of what’s called ‘muk’—a jelly-like food made from seaweed. It clogged the segment so severely that no content could pass. His intestine distended, his abdomen swelled, and he eventually vomited the contents, which refluxed into the lungs, causing fatal aspiration pneumonia.”
SBO Risk Flow in Elderly Patients
- ⬇️ History of abdominal surgery
- ⬇️ Adhesion formation → Intestinal narrowing
- ⬇️ Decreased mobility and muscle tone with age
- ⬇️ Intake of indigestible or sticky foods
- ⬇️ Reduced bowel movement efficiency
- ⬇️ Obstruction and intestinal swelling
- ⬇️ Vomiting → Aspiration → Respiratory failure
Prevention: What You Can Actually Do
Here’s what elderly individuals—and their caregivers—should prioritize:
- Regular, light exercise to promote gut motility
- Small, well-chewed meals—avoid sticky or fibrous food
- Hydration to reduce constipation risk
- Prompt checkups after any abdominal pain or irregular bowel movement
- Insurance coverage that includes gastroenterology services and ER access
“When you’re old, the margin of error is razor thin. One bad meal or one missed symptom can escalate fast.”
Why Insurance Is Your Best Protection
It’s tempting to think of insurance as just another monthly bill. But if you’ve read this far, you already understand:
Your intestines don’t ask for permission to get sick.
“Whether it’s Crohn’s, celiac disease, or an obstruction, the digestive system can turn on you with no warning. And the only thing worse than the pain—is the bill.”
Many patients think they’ll be able to pay as they go. But what happens when you need:
- A biologic injection costing $5,000 per dose?
- A hospital stay that runs $30,000+ in 3 days?
- Ongoing immune-modulating therapy for months or years?
- Nutritional counseling, lab tests, GI specialist consultations?
Suddenly, that “extra bill” becomes a lifesaver.
📊 [TABLE: Covered vs Not Covered – Outcomes]
| Scenario | With Insurance | Without Insurance |
|---|---|---|
| Diagnosed with Crohn’s Disease | Covered meds, GI follow-up, disability support | Delayed care, risk of bowel resection |
| SBO Emergency | ER + surgery covered, full recovery possible | Financial catastrophe or refusal of care |
| Routine GI Screening | Included in preventive care benefits | Often skipped → missed early warning signs |
What Kind of Plan Should You Look For?
If you suspect—or already manage—chronic digestive issues, you may want to consider:
- Silver or Gold tier ACA plans (lower deductibles, better specialist access)
- PPO plans (wider network for out-of-state emergencies)
- HSA-compatible high-deductible plans only if you have solid savings
- Medicaid or Medicare Advantage for eligible individuals with income limits or age 65+
📎 Compare Plans – Healthcare.gov
📎 Crohn’s & Colitis Financial Help
📎 SSDI & Digestive Disorders – SSA
“A good insurance plan won’t make you healthier. But it gives you a fighting chance when your health breaks down.”
Why Insurance Is Your Best Protection
It’s tempting to think of insurance as just another monthly bill. But if you’ve read this far, you already understand:
Your intestines don’t ask for permission to get sick.
“Whether it’s Crohn’s, celiac disease, or an obstruction, the digestive system can turn on you with no warning. And the only thing worse than the pain—is the bill.”
Many patients think they’ll be able to pay as they go. But what happens when you need:
- A biologic injection costing $5,000 per dose?
- A hospital stay that runs $30,000+ in 3 days?
- Ongoing immune-modulating therapy for months or years?
- Nutritional counseling, lab tests, GI specialist consultations?
Suddenly, that “extra bill” becomes a lifesaver.
📊 [TABLE: Covered vs Not Covered – Outcomes]
| Scenario | With Insurance | Without Insurance |
|---|---|---|
| Diagnosed with Crohn’s Disease | Covered meds, GI follow-up, disability support | Delayed care, risk of bowel resection |
| SBO Emergency | ER + surgery covered, full recovery possible | Financial catastrophe or refusal of care |
| Routine GI Screening | Included in preventive care benefits | Often skipped → missed early warning signs |
What Kind of Plan Should You Look For?
If you suspect—or already manage—chronic digestive issues, you may want to consider:
- Silver or Gold tier ACA plans (lower deductibles, better specialist access)
- PPO plans (wider network for out-of-state emergencies)
- HSA-compatible high-deductible plans only if you have solid savings
- Medicaid or Medicare Advantage for eligible individuals with income limits or age 65+
📎 Compare Plans – Healthcare.gov
📎 Crohn’s & Colitis Financial Help
📎 SSDI & Digestive Disorders – SSA
“A good insurance plan won’t make you healthier. But it gives you a fighting chance when your health breaks down.”