Think your cold symptoms are harmless? Think again. Discover the real dangers, how to protect yourself, and why U.S. health insurance still matters.
- Part 1. Cold Symptoms You Should Never Ignore: Why It’s More Than Just a Cold
- Part 2. What Actually Happens When You Catch a Cold
- Part 3. Why Over-the-Counter Drugs Might Delay Healing
- Part 4. How to Prevent Cold the Scientific Way
- Part 5. What Does Health Insurance Actually Cover for a Cold?
- Part 6. When to See a Doctor (and When Not To)
- Part 7. Prevention Strategies That Actually Work
- Part 8. What If It’s Not Just a Cold?
- Part 9. Final Takeaways & Cold Prevention Checklist
Part 1. Cold Symptoms You Should Never Ignore: Why It’s More Than Just a Cold
“You may not die from a cold, but you certainly can’t ignore it.”
— Dr. Samuel Lee, neurologist and medical researcher based in Boston
In America, the common cold is often dismissed as nothing more than an inconvenience — something to push through with a box of tissues and some over-the-counter meds. But according to Dr. Samuel Lee, who has spent years studying neurological responses to viral infections, this approach is dangerously outdated.
Most people don’t realize that what they call “just a cold” may actually be influenza, early-stage pneumonia, or a viral infection that taxes the immune system more than they think. More importantly, in a country where healthcare costs can exceed $300 for a single urgent care visit, brushing off cold symptoms without insurance could be a costly mistake — both for your health and your wallet.
Are You Sure It’s Just a Cold?
Dr. Lee recalls a time when he thought he had a bad cold, only to later realize it was actually the flu. The aches, the fever, the week-long recovery — all classic signs. But even as a trained physician, he didn’t recognize the difference until his own daughter was diagnosed with H1N1.
This is more common than you might think. The symptoms of colds and flu can overlap — congestion, sore throat, low-grade fever, fatigue — but the consequences can differ dramatically.
Real Cost of Misjudging Cold Symptoms in the U.S.
In the United States, here’s what you might pay out-of-pocket without health insurance:
| Service | Average Cost Without Insurance |
|---|---|
| Urgent Care Visit | $150 – $300 |
| ER Visit (non-emergency) | $500 – $2,000 |
| Chest X-Ray | $250 – $1,000 |
| Prescription Cold & Flu Meds | $30 – $120 |
“Healthcare in the U.S. doesn’t wait for a diagnosis to start billing.”
— Consumer Reports, 2022
Why Health Insurance Still Matters — Even for a Cold
Having health insurance — even a basic plan — can drastically reduce your financial burden. Many plans cover:
- Urgent care visits with low copays
- Telehealth consultations for cold and flu
- Generic medications
- Flu shots and preventative screenings
🔗 Check affordable options here:
👉 Compare Plans on eHealthInsurance
Part 2. What Actually Happens When You Catch a Cold
“Rhinoviruses replicate most efficiently at 91°F. That’s exactly what happens inside your nose while you’re asleep.”
— Dr. Samuel Lee
You might think catching a cold is as simple as “someone sneezed, and I got it.” But the biological reality is much more fascinating — and a little scary.
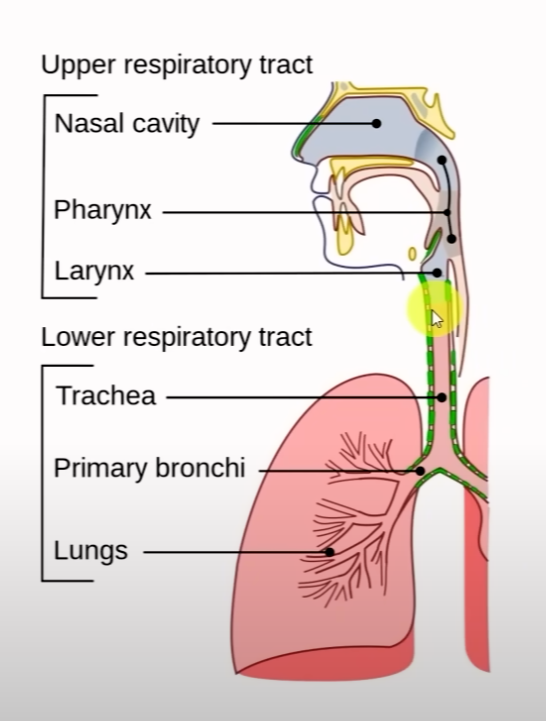
The most common culprit behind cold symptoms is rhinovirus, a microbe that loves cool, moist environments. And guess where in your body fits that description perfectly?
Your nasal passages, especially while you’re sleeping.
Why 91°F (32°C) Is a Virus’s Favorite Number
Here’s what happens on a cellular level:
- During the day, your body maintains a core temperature of around 98.6°F (37°C).
- But at night — especially when you’re resting, underfed, or in a cold room — the temperature inside your nose can drop to around 91°F (32°C).
- That’s when rhinoviruses become most active. They latch onto the cells in your nasal lining, multiply, and start overwhelming your immune system.
“We lose heat through the nose continuously. That’s where colds begin — not in your lungs or throat.”
— Harvard Health Blog
How Cold Viruses Enter and Multiply in Your Body
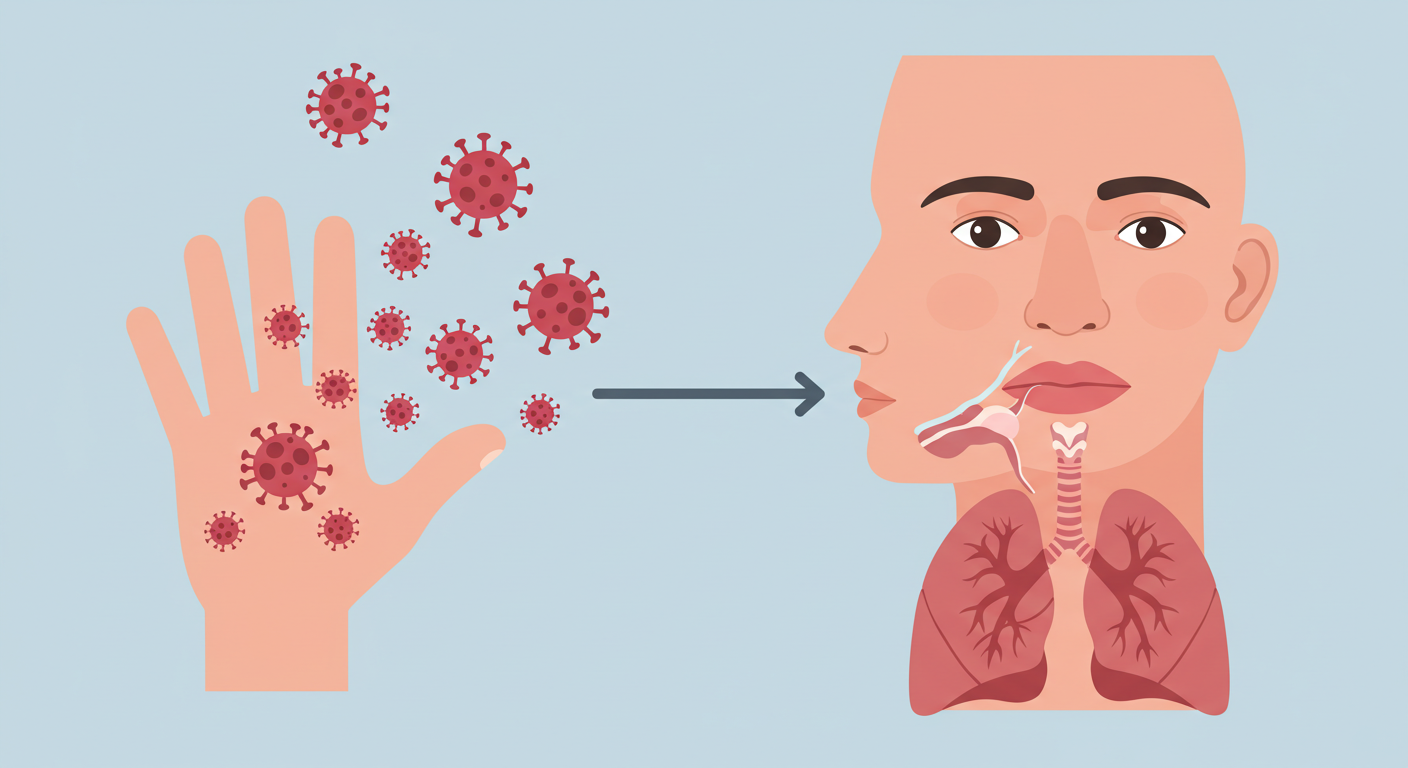
🦠 Viral Invasion Pathway
- Contact: You touch a contaminated doorknob or handshake.
- Transfer: You touch your nose, eyes, or mouth.
- Attachment: Virus binds to nasal lining (cooler than body temp).
- Replication: Virus hijacks your cells to multiply.
- Symptoms: Your immune system fights back — leading to congestion, sore throat, fever.
So What Can You Do?
- Keep warm while sleeping, especially your neck and upper chest.
- Avoid sleeping in cold, dry rooms — consider a humidifier.
- Hydrate well before bed to support immune function.
- Nasal rinses can help wash away viruses before they replicate.
Insurance Tip: Telehealth Can Help You Catch It Early
Many health insurance plans now include telehealth consultations. If you start to feel cold symptoms, don’t wait. A quick virtual visit can:
✔️ Confirm whether it’s a cold or something more serious
✔️ Provide a prescription for relief (if needed)
✔️ Document the case for insurance purposes
🔗 Explore telehealth-enabled plans:
👉 Get Instant Quotes with Telehealth Included
Part 3. Why Over-the-Counter Drugs Might Delay Healing
“Fever, fatigue, congestion — they’re not just symptoms. They’re your body fighting back.”
— Dr. Samuel Lee
When most Americans get cold symptoms, their first instinct is to reach for the medicine cabinet. Acetaminophen for fever. Antihistamines for congestion. Maybe a decongestant spray, cough suppressant, and multivitamin.
But here’s the surprising truth: taking over-the-counter (OTC) medication too early or too often might actually delay your recovery.
What Cold Medicines Are Really Doing
Your body responds to viral infections by triggering fever, inflammation, and mucus production. These uncomfortable symptoms are not the virus itself — they’re your immune system fighting back.
“Fever is your internal alarm system. It activates immune cells to work faster.”
— Journal of Immunology, 2021
So when you take medications that:
- Lower your fever (e.g., Tylenol)
- Suppress your cough (e.g., Dextromethorphan)
- Dry out your nose (e.g., Diphenhydramine)
…you might feel better, but your immune system may be getting less support than it needs.
Scientific Insight: Energy Allocation in Your Body
Your body allocates energy in priority order:
- Basal metabolism (just staying alive)
- Movement and muscle activity
- Immune function
When you’re sick, your body tries to divert more energy to immune response. But if you:
- Diet too hard
- Overexert yourself
- Suppress symptoms prematurely
…you might be interfering with your body’s natural healing order.
Common Cold Medications vs. Immune Impact
| Medication Type | Example | Effect on Body | Immune Impact |
|---|---|---|---|
| Antipyretic | Acetaminophen (Tylenol) | Reduces fever | May slow immune activation |
| Antihistamine | Diphenhydramine (Benadryl) | Reduces nasal discharge | Suppresses mucus — a virus-clearing tool |
| Cough Suppressant | Dextromethorphan | Suppresses cough reflex | May inhibit clearing of virus-laden fluids |
What Health Insurance Covers — and What It Doesn’t
Most U.S. health insurance plans don’t cover OTC medication, even if it’s recommended by a doctor. However, many will cover:
- Telehealth consults to verify if it’s cold or flu
- Prescription medications if needed
- Diagnostic tests (like COVID-19, influenza)
- Urgent care visits if symptoms worsen
💡 Tip: Use Health Savings Accounts (HSAs) or Flexible Spending Accounts (FSAs) to cover OTC drugs tax-free if not reimbursed.
🔗 Explore plans with telehealth and Rx coverage:
👉 Shop Smart Health Plans on Policygenius

Part 4. How to Prevent Cold the Scientific Way
“Cold viruses are always around. The key is not eliminating them — it’s outsmarting them.”
— Dr. Samuel Lee
Most people treat a cold after symptoms show up. But what if you could stop it before it takes hold?
Research shows that rhinoviruses, the leading cause of cold symptoms, begin replicating rapidly when:
- Your nasal temperature drops to around 91°F (32°C)
- Your immune energy is low (due to fatigue, undernourishment, or stress)
- You’re exposed via contaminated surfaces or airborne particles
So instead of waiting to feel miserable, you can build a daily routine that blocks the virus before it gains a foothold.
7-Day Scientific Cold Prevention Plan
| Day | Preventive Action | Why It Works |
|---|---|---|
| Day 1 | Use a humidifier at night | Keeps nasal passages moist, makes virus replication harder |
| Day 2 | Do a saline nasal rinse before bed | Washes out virus particles before they attach to cells |
| Day 3 | Disinfect phone, glasses, and doorknobs | Reduces hand-to-face transfer of viruses |
| Day 4 | Wear a neck warmer while sleeping | Helps maintain nasal temperature above 91°F |
| Day 5 | Gargle after coming home | Flushes viruses from the throat before replication |
| Day 6 | Take warm fluids (tea, soup) before bed | Boosts core temperature and hydration |
| Day 7 | Sleep 7–9 hours in thermal pajamas | Supports immune recovery and prevents nasal cooling |
U.S. Health Insurance and Preventive Benefits
Many people don’t realize that most U.S. health insurance plans cover cold prevention services, including:
- ✔️ Annual flu shots (100% covered under ACA-compliant plans)
- ✔️ Telehealth screening visits at $0–$40 copay
- ✔️ Preventive counseling on immunity and respiratory care
- ✔️ COVID-19 & Influenza testing
🔗 Check which plans include preventive coverage:
👉 Healthcare.gov – Compare Covered Benefits
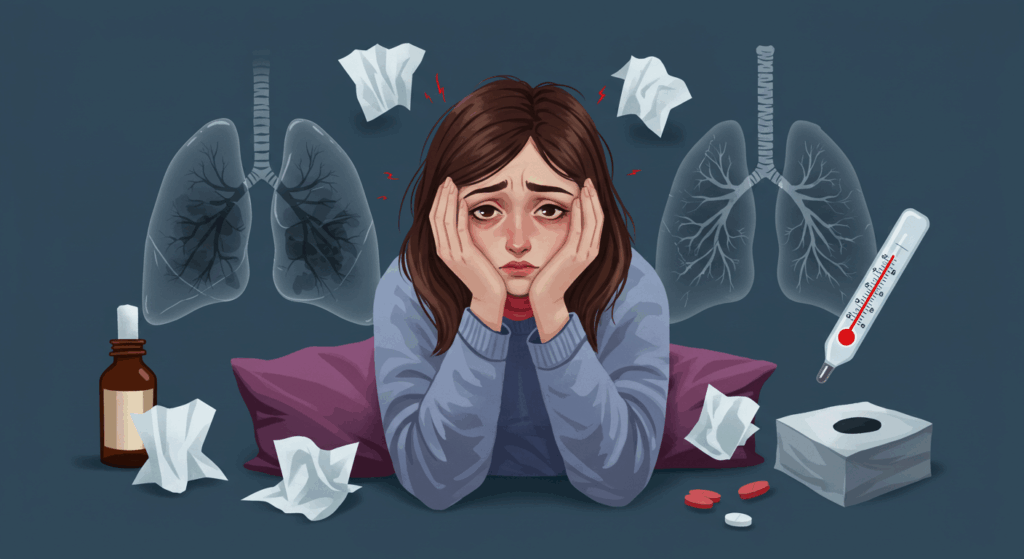
Part 5. What Does Health Insurance Actually Cover for a Cold?
“Feeling sick is stressful enough. The last thing you need is surprise medical bills.”
— National Health Council
You Have Cold Symptoms — What Now?
Imagine this: You’ve had a sore throat and runny nose for 3 days. It’s not going away. You’re wondering if it’s just a cold or something worse.
Here are your options in the U.S., and what they typically cost depending on your insurance:
Medical Options & Costs by Insurance Type
| Service Type | Insured (PPO) | Insured (HMO) | Uninsured |
|---|---|---|---|
| Telehealth Visit | $0–$40 copay | $0–$20 copay (in-network) | $59–$90 per session |
| Urgent Care | $30–$100 | $25–$75 (referral often needed) | $150–$250 avg. |
| Emergency Room (ER) | $200–$500 copay + deductible | Only if referred or life-threatening | $600–$1,500 avg. |
| Prescription Medication | Covered (generic: $5–$15) | Covered (usually free generics) | $20–$100 full price |
For Uninsured Individuals
If you don’t have insurance, here’s what you can do:
- ✔️ Use retail clinic chains like CVS MinuteClinic or Walgreens (basic cold care for $89–$129)
- ✔️ Use GoodRx or SingleCare to get prescription discounts
- ✔️ Visit community health centers — often income-based pricing
- ✔️ Consider short-term emergency medical insurance for 30–90 days
👉 Explore temporary plans on Agile Health
“One of the most affordable cold-related visits is a telehealth consultation. Even for the uninsured, it often costs under $60 and can save a $250+ urgent care bill.”
✔️ PPO Plan
- 🏠 Home symptoms
- ➡️ Telehealth ($0–$40)
- ➡️ Urgent Care ($30–$100)
- ➡️ Emergency Room ($200+)
- 💊 Prescription: Covered ($5–$15)
📋 HMO Plan
- 🏠 Home symptoms
- ➡️ In-network Telehealth ($0–$20)
- ➡️ Referral needed → Urgent Care
- ➡️ Emergency Room (if approved)
- 💊 Prescription: Often free
❌ Uninsured
- 🏠 Home symptoms
- ➡️ Telehealth ($59–$90)
- ➡️ Urgent Care ($150–$250)
- ➡️ Emergency Room ($600+)
- 💊 Prescription: Full price ($20–$100)
Part 6. When to See a Doctor (and When Not To)
How to Know When It’s “Just a Cold”
Not every sniffle needs a doctor.
If you’re experiencing symptoms like:
- Runny or stuffy nose
- Sore throat without fever
- Mild fatigue
- Occasional cough
- No shortness of breath or chest pain
…then you’re likely dealing with a common cold. These symptoms are manageable at home using:
- Rest and hydration
- Over-the-counter medications (like acetaminophen or ibuprofen)
- Warm fluids and humidifiers
“If your symptoms don’t worsen after 3 days, it’s likely self-resolving.”
— American Lung Association
✔️ If you have insurance:
Use your telehealth benefits first. Most PPO or HMO plans now include free or low-cost virtual consultations.
❌ If you’re uninsured:
Try services like PlushCare or GoodRx Care for one-time telehealth visits ($39–$89).
Red Flags: When It’s NOT Just a Cold
If you’re experiencing any of the following, it’s time to see a doctor immediately:
- Fever over 102°F (38.9°C)
- Shortness of breath
- Persistent chest pain
- Green/yellow mucus for more than 7 days
- Severe headache or neck stiffness
These symptoms may indicate something more serious like flu, pneumonia, sinus infection, or even COVID-19.
“Chest pain accompanied by high fever is never just a cold.”
— Mayo Clinic
✔️ Insured?
Most plans will cover urgent care visits or ER if symptoms meet criteria.
❌ Uninsured?
Look for low-cost community clinics like FindHealthCenter or walk-in clinics (often $100–$250).
Doctor Visit Costs: With vs Without Insurance
| Service | With Insurance | Without Insurance |
|---|---|---|
| Telehealth | $0 – $40 | $39 – $90 |
| Urgent Care Visit | $30 – $100 | $150 – $250 |
| ER Visit | $100 – $300 | $600 – $1,500+ |
Insurance Tip: Affordable Options You Should Know
Don’t wait until you’re sick to figure this out.
If you qualify for Medicaid, check your eligibility instantly via Healthcare.gov.
If not, browse affordable marketplace plans on:
- HealthSherpa
- Stride Health
- Covered California (California residents only)
Part 7. Prevention Strategies That Actually Work
Why Prevention Matters More Than Cure
Preventing a cold is much cheaper—and safer—than treating one.
For uninsured individuals, a single ER visit can cost over $1,000. But most colds can be avoided with a few simple habits.
“An ounce of prevention is worth a pound of cure.”
— Benjamin Franklin
✔️ Avoiding a cold protects not just your health, but also your wallet.
What Actually Works (Backed by Data)
| Prevention Strategy | Effectiveness |
|---|---|
| Washing hands frequently | ⬆ Reduces cold transmission by up to 45% |
| Avoiding face touching | ⬆ Breaks contact transmission path |
| Proper sleep & nutrition | ⬆ Supports immune system response |
What Doesn’t Work (But People Still Believe)
“Vitamin C prevents colds!”
Not really. Studies show it doesn’t reduce your chance of getting sick, but may shorten symptoms slightly.
“Going out with wet hair causes colds.”
False. Colds are caused by viruses, not temperature or hair moisture.
Does Insurance Cover Preventive Measures?
Yes—many insurance plans, including ACA-compliant ones, cover:
- Annual wellness exams
- Flu shots
- Preventive counseling (e.g., smoking cessation, nutrition)
If you’re not covered, check these resources:
Cold Prevention Flow
Wash Hands
Avoid Touching Face
Boost Immunity
Part 8. What If It’s Not Just a Cold?
When a Cold Becomes Something More Dangerous
Sometimes what feels like an ordinary cold is actually a sign of something more serious—like sinusitis, bronchitis, or even pneumonia. Especially if you’re uninsured, delaying a doctor visit can put you at real risk.
“I thought it was just a cold… until I was hospitalized for pneumonia.”
— James M., 42, Philadelphia
Symptoms That Should Never Be Ignored
- Persistent fever over 102°F
- Shortness of breath
- Chest tightness or pain
- Green or yellow mucus for more than a week
- Confusion or dizziness
“Most ER doctors agree: breathing difficulty + fever is a red flag.”
— Emergency Medicine Journal
Why Insurance Can Be a Life-Saver Here
| Medical Scenario | With Insurance | Without Insurance |
|---|---|---|
| Emergency Room Visit | $100–$300 copay | $1,500–$3,000 full cost |
| Chest X-ray | Covered (with referral) | $300–$600 |
| Antibiotic treatment | $10–$40 | $80–$200 |
Insurance Recommendations
If you’re uninsured or worried about surprise bills:
- 👉 Consider a Bronze ACA plan if your income qualifies
- 👉 Look into Short-Term Health Insurance via:
- 👉 Visit HealthCare.gov to check open enrollment or Medicaid eligibility
“Being uninsured nearly tripled the risk of avoiding emergency care due to cost.”
— Journal of Health Affairs, 2022
Part 9. Final Takeaways & Cold Prevention Checklist
Summary: What We’ve Learned So Far
✔️ Colds are viral—not bacterial—and most don’t need antibiotics
✔️ Prevention is far more cost-effective than treatment
✔️ Without insurance, even a mild illness can trigger major financial risk
✔️ Some symptoms should never be ignored
“Getting sick isn’t always your choice. But being prepared always is.”

Cold Prevention & Readiness Checklist
| To-Do | Status |
|---|---|
| Wash hands regularly | ☐ |
| Avoid face touching | ☐ |
| Stay home when sick | ☐ |
| Get annual flu shot | ☐ |
| Have active health insurance | ☐ |
Final Note: You Don’t Need to Face It Alone
“The best time to get insured was yesterday. The second-best time is now.”
Still uninsured? Don’t wait until you’re sick.
Visit HealthCare.gov or compare private plans here:
- eHealthInsurance (VPN may be required in some regions)
- PolicyGenius
- HealthSherpa
I Got a $1,770 ER Bill One Year Later — What You Need to Know About Out-of-Network Charges
Emergency care might feel urgent, but your insurance might not agree. Here’s how to appeal…
Why Good Sam RV Insurance Is the Top Choice for RV Owners in America
Find out why thousands of RVers trust Good Sam for total loss replacement, full-timer coverage,…
Can You Really Use Home Insurance Claim Money for Something Else?
Wondering if you can use your home insurance claim for a different repair? We break…
What to Do When an Unauthorized Driver Hits You in a Rental Car Accident
Got hit by an unauthorized driver in a rental car and left with unpaid bills?…
I Woke Up With No Memory, Vomiting, and Two Pairs of Underwear — What Happened to Me?
She woke up sick, confused, and with no memory — her clothes were changed, her…
When a Developer Demands You Move Your Mailbox: A Houseowner’s Stand Against Unfair Pressure
A developer told a rural houseowner to move their mailbox to make way for a…